/ Research, Studies
Fighting brain cancer (Hutter Lab)
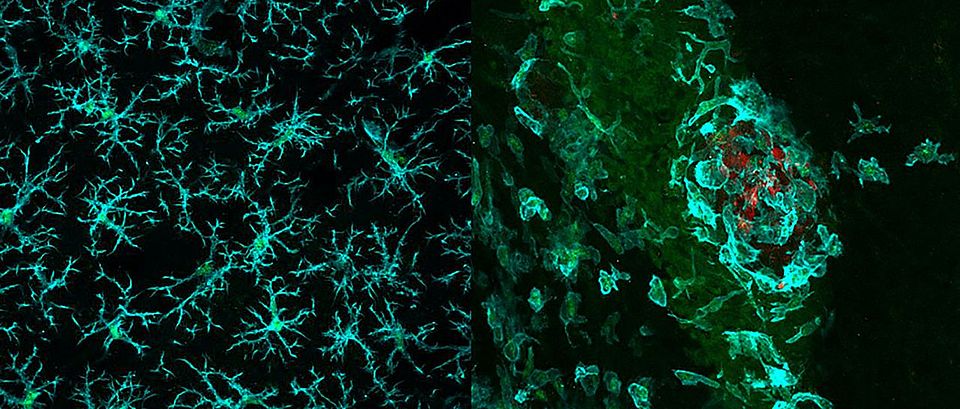
Fluorescence microscopic image of stained tissue sections (mouse). Left: Macrophages (green) in normal brain tissue. Right: Macrophages (green) attacking a tumor (red). (Image: Dr. Marie-Françoise Ritz, University of Basel, Department of Biomedicine, and Nicoletta Ferrari, LMU University Hospital, LMU Munich)
Glioblastomas are among the most aggressive kinds of brain tumors. Even immunotherapy treatments that have proved effective against other cancers seem to be powerless against them. Researchers at the University of Basel and University Hospital Basel have now described how to improve the immune system’s chances against this type of tumor.
“Don’t eat me!” That’s how one might translate the signal that the cancer cells in a glioblastoma send to the macrophages (white blood cells specialized in removing dead and dying cellular matter) in the brain. Immunotherapy attempts to enable these cells to eradicate the abnormal cells, but so far, it has met with little success when it comes to glioblastomas.
Researchers led by Professor Gregor Hutter from the Department of Biomedicine at the University and University Hospital Basel have recently used patient data, experiments with mice, and samples from human tumors to study one of these “don’t eat me!” signals and its inhibitory effect. Their findings, which may pave the way for effective immunotherapies for glioblastomas, are now being published in Science Translational Medicine.
The signal is based on sugar molecules called sialic acid glycans on the surface of the cancer cells. These sugar molecules are recognized by “receivers” on the surface of the brain’s macrophages and interpreted as “don’t eat me!” Hutter’s team of researchers reports that patients whose macrophages have especially high numbers of these “Siglec9” receivers have a lower survival rate.
Turning off the receiver
When the researchers used a genetic trick to remove the mouse variant of Siglec9 from the brain macrophages of laboratory mice, brain tumors in these mice grew significantly more slowly. One indicator that the macrophages were able to partly hold the glioblastoma at bay: they no longer had the receiver that allowed them to perceive the “don’t eat me!” signal, so they were able to proceed with their task of removing the abnormal cells. The researchers also saw the same effect when they implanted tumor cells that did not have any sugar molecules on their surface.
They confirmed this in experiments with surgically-removed brain tissue from glioblastoma patients, which the researchers cultivated in the lab. If they gave the cultivated cells an antibody that blocked the Siglec9 receiver, they were able to observe an activation of the immune cells in the tumor and the directly adjacent tissue.
“Taken together, our results suggest that the sialic acid-Siglec axis could be a promising therapeutic target,” Hutter explains. If the receivers on patients’ macrophages could be switched off with antibodies, existing immunotherapies might be able to take full effect against glioblastomas as well. The next step in the team’s research is to examine in clinical studies whether it is possible to provide a local dose of antibodies against the receiver in the brain and whether this has the desired effect.
Social Media
