Cartilage Repair - The Problem

Cartilage tissue has a limited capacity for self-repair and does not heal by itself. If left untreated, this can lead to an increased risk of osteoarthritis. Click here to read more about current treatments and our innovative still experimental strategy.
Cartilage tissue has a limited capacity for self-repair. Articular cartilage injuries that are not properly treated cause pain and disability, and double the incidence of degenerative joint problems in the elderly. Cartilage repair treatments do have the potential to relieve pain and improve the quality of life for younger patients as well as slowing down or eliminating the need for joint replacement in the older patient.
Common current treatment strategies such as arthroscopic debridement, microfracture, transplantation of allografts or autologous osteochondral grafts suffer from major drawbacks such as defect-size limitations, donor-site morbidity and limited graft material. Established cell-based techniques, using exclusively articular chondrocytes, such as autologous chondrocyte implantation (ACI) show generally good clinical results. Major drawbacks are that this technique is not indicated for older patients and has limited efficacy in degenerative disease.
We hope to overcome these drawbacks by using an innovative cell source (nasal chondrocytes), which have a higher capacity to form cartilage in older patients. Furthermore, these cells are implanted as a tissue engineered nasal cartilage graft as compared to only cells, which makes them more resilient to inflammatory environment usually seen in degenerative disease. We believe that this will lead to a repair tissue with comparable properties to native cartilage and thus to a more durable repair in the long-term.
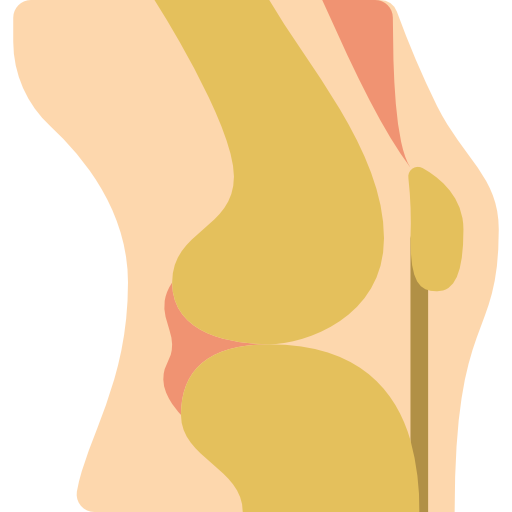
Knee osteoarthritis is one of the most common causes of pain and limited mobility. It makes everyday activities difficult or impossible and significantly reduces the quality of life of those affected. More than 260 million people worldwide suffer from osteoarthritis. Increase in life expectancy and the rising proportion of overweight people will cause the numbers to rise even further in the future.
Current treatments are limited to medication for pain, symptom relief, correction of deformities or - in the final stage - the use of an artificial knee joint. Although the latter generally shows satisfactory results, complications can occur. 10-15% of patients are dissatisfied with the results of the treatment. Especially in patients below 60 years of age, delaying an artificial knee joint is important, because satisfaction with the treatment is lower and the risk of having a second replacement surgery in the course of one's life is significantly increased. Knee osteoarthritis often begins with what is known as patellofemoral osteoarthritis (PFOA), extensive cartilage damage behind the kneecap that can then progress to generalized osteoarthritis. A novel therapy based on the body's own nasal cartilage cells could not only alleviate the symptoms of PFOA in this case, but also slow down or prevent progression of the disease. This therapy may be an important alternative for those who are too young for an artificial knee joint intervention, but who can no longer manage their life with painkillers alone.
arthroscopic debridement: Procedure of removing damaged cartilage and tissues in a minimally invasive surgery
articular chondrocytes: Chondrocytes (cartilage cells) from the joint.
autologous chondrocyte implantation (ACI): Cartilage cells are harvested from the knee of the patient, expanded in a laboratory and re-implanted in the cartilage defect of the same patient to heal the defect.
autologous osteochondral grafts: Cartilage/bone tissue is harvested in a non-load bearing site of the knee of the patient and transplanted to the cartilage defect. Autologous = from your own body
donor-site morbidity: Diseases developing at the site of harvesting of the tissue
microfracture: Procedure of creating tiny fractures or holes in the bone to induce bleeding and thus attract bone marrow stem cells to the surface to form a repair tissue for the cartilage.
second-generation Matrix-assisted ACI (MACI): Cartilage cells are harvested from the knee of the patient, expanded in a laboratory and seeded onto a scaffold to adhere to it. The scaffold together with the cells is then implanted in the cartilage defect of the same patient.
transplantation of allografts: Cartilage/bone tissue is transplanted from a deceased person to the patient to repair the cartilage defect
